What Does Indigestion Feel Like?
Indigestion can feel like:1,2
- Feeling too full after eating or being unable to finish a meal because you feel full
- Pain or burning in the upper region of your stomach
- Nausea or heartburn
- Bloating
- Burping

What Causes Indigestion?
Triggers for indigestion may differ from person to person and can include:4-10
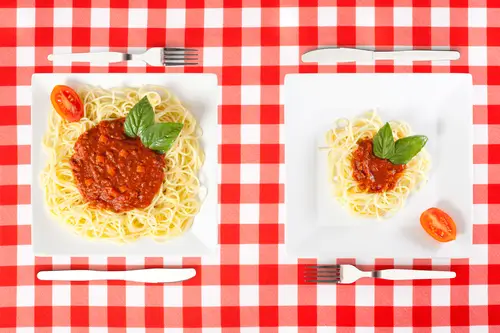
- Eating big meals and overfilling your stomach

- Pregnancy - hormonal changes and/or the pressure put on the stomach and
digestive tract by a growing baby

- Being overweight
- Smoking
- Certain medications
- Stress

Foods That Can Trigger Indigestion
Possible triggers of indigestion include:6,7
- Eating fatty foods, spicy foods, chocolate, mint or tomato products
- Drinking caffeinated drinks, alcohol or citrus juices
The Way You Eat
Ways you can help relieve or prevent indigestion include making changes to the way you
eat, such as:7,8
- Avoiding or limiting food and drinks that can trigger your symptoms
- Eating smaller meals
- Waiting 2 to 3 hours after eating or drinking before lying down
How Can I Help Relieve Indigestion At Home?
Aside from eating a healthy, balanced diet and minimising trigger foods as well as altering
how much and when you eat, there are also some over-the-counter products that may
help.
Medication like Gaviscon Dual Action contains both an antacid and alginate to help relieve
indigestion in two ways.
- The antacid – the antacid in Gaviscon Dual Action neutralises excess
stomach acid to relieve the pain and discomfort of indigestion.11 - The raft – the sodium alginate in Gaviscon Dual Action forms a thick layer
(think of it like a ‘raft’) on top of your stomach contents. The ‘raft’ then acts as
a physical barrier that helps keep your stomach contents where they belong11–
in your stomach – and not in your food pipe where they can cause discomfort
and burning pain4.
Complications
Whilst indigestion alone may not lead to serious complications, it can impact your day-to-day life. People suffering from indigestion long term may experience disturbed sleep, which can in turn affect how productive you are at work or school. Lack of sleep can also affect your mental health and wellbeing.12,13
If your symptoms do not resolve or if your symptoms are troubling or concern you, speak to your doctor.
Always read the label and follow the directions for use.
FAQs
This article is for general information only and not intended as a substitute for medical advice. All information presented on these web pages is not meant to diagnose or prescribe. In all health-related matters, always consult your healthcare professional.
Always read the label and follow the directions for use. RKT-M-27035.
References:
- Talley NJ, et al. Aust Prescr 2017;40:209–13.
- American Family Physician. Am Fam Physician 2010;82(12):1459–1460.
- Therapeutic Guidelines March 2020 edition. Functional gastrointestinal disorders. Available at: https://tgldcdp.tg.org.au (accessed July 2020).
- Better Health Channel. Indigestion. Available at: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/indigestion (accessed July 2020).
- Department of Health (2019) Clinical Practice Guidelines: Pregnancy Care. Canberra: Australian Government Department of Health. Part I:56 Reflux (heartburn).
- World Gastroenterology Organisation. WGO Handbook on HEARTBURN: A Global Perspective. 2015.
- Australian Medicines Handbook. Dyspepsia. Available at: https://amhonline.amh.net.au/ (accessed July 2020).
- Therapeutic Guidelines March 2020 edition. Disorders of the oesophagus: Gastro-oesophageal reflux. Available at: https://tgldcdp.tg.org.au (accessed July 2020).
- Sandhu D, Fass R. Proc Shevchenko Sci Soc Med Sci 2018;52:10–15.
- Cho YK. J Neurogastroenterol Motil 2017;23:526–532.
- Mandel KG, et al. Aliment Pharmacol 2000;14:669-690.
- Wuestenberghs F, et al. Front Neurosci 2022;16:829916.
- Matsuzaki J, et al. United European Gastroenterol J 2018;6(3):398–406.